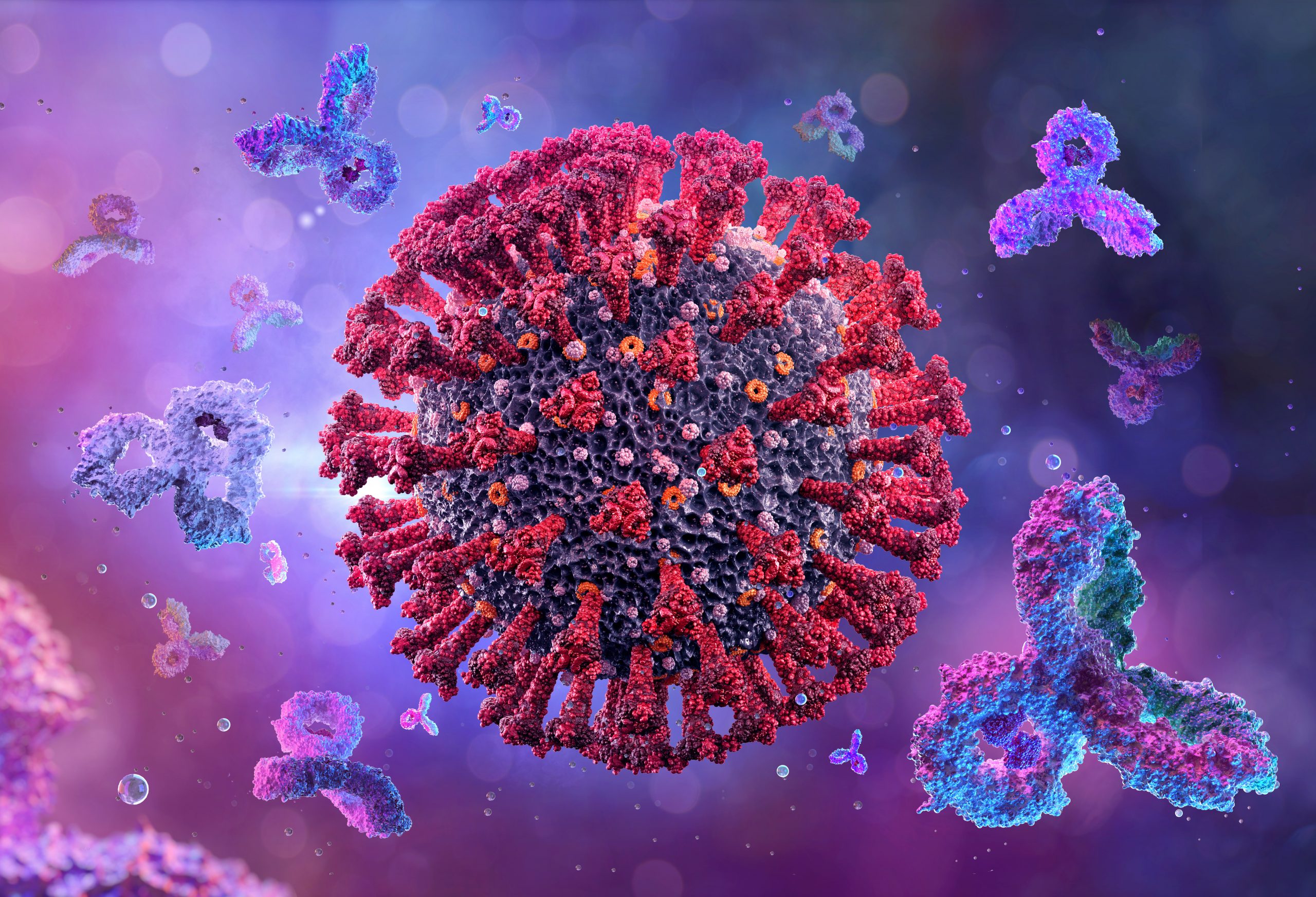
Scientists explore effectiveness of neutralizing antibodies against SARS-CoV-2 Omicron variant.
In
a recent study published in the Journal
of Experimental Medicine, researchers assessed the impact of severe acute
respiratory syndrome coronavirus 2 (SARS-CoV-2)-neutralizing antibodies on the SARS-CoV-2
Omicron variant.
Researchers around the world have explored
the development of vaccines and therapies to prevent and treat coronavirus
disease 2019 (COVID-19). Various studies are also investigating the
effectiveness of SARS-CoV-2-neutralizing antibodies-based immunotherapies, which
has led to the usage of several monoclonal antibodies (mAbs) against
COVID-19.
About
the study
In the present study, researchers reported
the functional and molecular characteristics of human SARS-CoV-2 spike (S) mAbs
derived from immunoglobulin G (IgG) and IgA memory B cells.
The team estimated the seroreactivity of
IgG and IgM in convalescent persons who had tested COVID-19 positive in the
first wave of infections to the SARS-CoV-2 Wuhan trimeric spike (tri-S) and
receptor-binding domain (RBD) proteins via enzyme-linked immunosorbent assay
(ELISA). The researchers also assessed the neutralizing activity of the IgG and
IgA antibodies found in the purified serum samples against the SARS-CoV-2 Wuhan
strain using an in vitro pseudoneutralization assay.
Furthermore, the team selected convalescent
persons to obtain peripheral blood IgG and IgA memory B cells which were
stained using fluorescently labeled tri-S and RBD. SARS-CoV-2 tri-S was used as
bait in order to capture singular SARS-CoV-2-reactive B cells via cytometric
sorting. From the SARS-CoV-2 tri-S IgG and IgA memory B cells isolated, the
team developed unique human mAbs from selected B cells as recombinant IgG1
antibodies. Subsequently, ELISA and binding analyses based on flow cytometry
were performed.
Results
The study results showed that the
serological samples obtained from convalescent individuals who had a history of
SARS-CoV-2 infection during the first wave of the pandemic exhibited high
titers of anti-tri-S IgGs, primarily IgG1. These titers also included
antibodies that cross-reacted against the Middle East respiratory
syndrome-related coronavirus (MERS-CoV) tri-S protein. The team also observed
high concentrations of serum anti-RBD IgGs, which were associated with
anti-tri-S antibody titers.
A correlation was found between the
SARS-CoV-2 seroreactivity of the IgG and the IgA antibodies. Serum IgG and IgG
antibodies obtained from patients having the highest anti-SARS-CoV-2 tri-S
antibody titers displayed robust ELISA binding to the SARS-CoV-2 Wuhan
nucleocapsid (N), RBD, and the tri-S, S1, and S2 subunits. These antibodies
also had a cross-reaction against recombinant S proteins belonging to other
beta-CoV such as SARS-CoV-1 and MERS-CoV.
The in vitro pseudoneutralization assay
showed that the 50% inhibitory concentrations (IC50) of the purified IgA
antibodies were lower than that of IgG antibodies. Moreover, the IC50 values of the IgA
antibodies were substantially inversely correlated to the respective binding
levels exhibited by the SARS-CoV-2 RBD and S1 proteins.
Binding analyses showed that 76% of the
purified mAbs selectively bound to the SARS-CoV-2 spike protein while
RBD-binding cells comprised 11% tri-S IgA and 17% tri-S IgG B cells.
Furthermore, anti-RBD IgA titers were inversely correlated with the IC50 neutralization
values for IgAs and directly proportional to the blood RBD IgA B-cell
frequencies. The team also noted that some antibody clones were present in
several COVID-19 convalescent individuals, suggesting the existence of
inter-individual convergence of anti-SARS-CoV-2 antibody responses.
Epitope mapping analyses performed by ELISA
using recombinant proteins revealed that almost 59% of the anti-S mAbs efficiently
bind to the S2 subunit, 17% to the N-terminal domain (NTD), 1% to the S1
connecting domain (CD), and 7% to other regions present in the SARS-CoV-2 S
protein. Approximately 0.99% of the total anti-S antibodies that targeted S2
recognized the tri-S protein but did not bind to the spike-covering linear
peptides, indicating that several SARS-CoV-2 spike memory B-cell antibodies
targeted conformational epitopes.
Notably, the antibodies Cv2.1169 and
Cv2.3194 exhibited a reduced neutralization efficiency against the SARS-CoV-2
Omicron BA.1 sublineage as compared to the SARS-CoV-2 Delta variant. On the
other hand, Cv2.1169 and Cv2.3194 displayed comparatively stronger RBD-binding
against the Omicron BA.2 sublineage than BA.1. The two antibodies showed efficient
blocking of BA.2 RBD-binding to angiotensin-converting enzyme-2 (ACE-2).
Overall, the study
findings showed that antibodies Cv2.1169 and Cv2.3194 exhibited robust
neutralizing activity against SARS-CoV-2 Omicron BA.1 and BA.2 and were found
to be the most potent cross-neutralizer used clinically against COVID-19. The
researchers believe that these antibodies could serve as potential candidates
in the development of prophylactic as well as therapeutic approaches against
SARS-CoV-2 infections.